Health equity is often referred to as “the highest level of health for all people,” and achieving health equity often requires addressing health disparities related to social and economic factors, including conditions in which people are born, grow, live, work and age.
While access to health care is incredibly important, the social determinants of health “include living and working conditions, education, income, neighborhood characteristic, social inclusion and medical care,” according to the Robert Wood Johnson Foundation.
Things like quality schools and housing, access to good jobs and healthy food, and safety of our neighborhoods play a role in overall health. Unfortunately, everyone doesn’t have access to these things and it plays into how healthy they are or how long they live.
When we remove barriers to health, like poverty, discrimination, racism and promote improved access to health care, good jobs, quality education, housing, or safe environments, that’s when all people can attain their highest level of health.
Data spotlights inequities for specific population groups or by geographic location, which helps the Kansas Health Foundation (KHF) determine priorities and allocate resources most effectively. Even with the coronavirus disease (COVID-19) pandemic, data indicated older adults, people of color and those with disabilities were disproportionately affected by COVID-19.
Seeing these growing challenges for underserved communities, our late CEO Reggie Robinson set the vision for us to do more, to be more deliberate and intentional about our work, using a health equity lens. We believe our first step is sharing more about the disparities so it’s clear about the “why and for whom” of our KHF work, and the opportunities that lie ahead.
What Health Disparities Look Like
With an understanding of the basic concept of health equity, it’s important to examine a few measures of health disparities in Kansas, including income, race and geography.
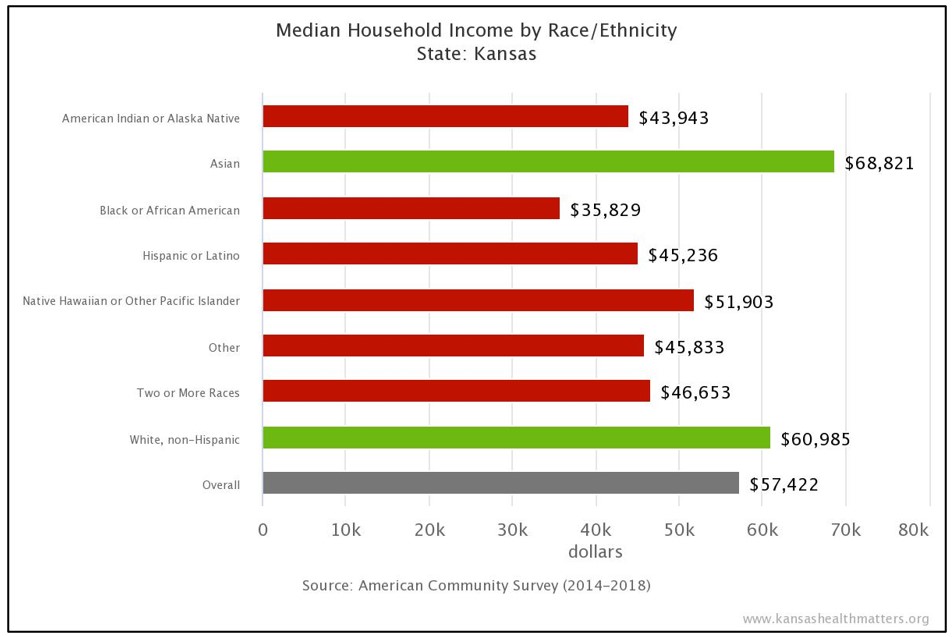
According to the American Community Survey from March 2020, the median household income for most minority Kansans is significantly less than that of white households (as seen in the chart to the right).
Income levels affect so many social determinants of health and the ability to access basic needs for healthy daily life. For example, access to health care is often unaffordable for many lower income Kansans.
Kansans of racial/ethnic minorities are more likely to be uninsured than white Kansans (15.2 percent versus 6.6 percent, respectively), with Hispanics having the highest likelihood of being uninsured at 21.7 percent, according to Kansas Health Institute (KHI) analysis of data from the U.S. Census Bureau 2018 American Community Survey.
Uninsured rates among Kansans age 19-64 are higher in Southwest Kansas counties (20.2 percent) than in Northeast Kansas (10.9 percent) or the second highest uninsured region of South Central Kansas (13.6 percent), according to KHI analysis of the U.S. Census Bureau 2018 Small Area Health Insurance Estimates.
These disparities have increased during the COVID-19 pandemic as more Kansans lost jobs and health care coverage. The pandemic has caused disproportionate impacts to minority and low-income populations.
This was apparent when remote learning and telemedicine became the norm, as many Kansans and communities did not have adequate internet access, primarily due to affordability or lack of community infrastructure.
There is an increasing need for adequate internet access, which is required for telehealth, education, business and social activities, according to KHI’s latest 2021 report on Kansas internet access.
- Overall, three in 10 (29.8 percent or 884,700) Kansans lacked adequate internet access in 2019 (device availability and high-speed internet connection). Regions with the greatest rates of inadequate internet access included East Central Kansas (44.7), Southeast Kansas (43.6 percent) and Southwest Kansas (42.7 percent).
- Kansans who are non-Hispanic Black or Hispanic were more likely to lack adequate internet access than were non-Hispanic White Kansans (45.6 percent, 39.8 percent and 28.5 percent, respectively).
- One in four (26.7 percent) Kansas children live in households that lacked adequate internet access, possibly making remote learning difficult for school-aged children.
- Older adults were most likely to lack adequate internet access (43 percent) as were those with a functional disability (43.2 percent).
Without proper access to internet, it’s hard for these individuals to receive the proper health care, education or social activities needed to succeed.
While these examples of inequities affect all aspects of daily life, KHF knows they only tell part of the story.

KHF’s Health Equity Work
For several years, KHF has intentionally allocated resources to help address health disparities. For the past seven years we have continued to support Medicaid expansion, which would bring greater access to affordable health care for more than 130,000 low-income Kansans. Helping people access early preventive health services reduces the crippling effect of costly and more serious illness later.
The “Can’t Wait to Read” literacy campaign was strategically focused in eight school districts experiencing the highest rates of free- and reduced-price lunch and racial/ethnic diversity. Additional grants to support the Dolly Parton’s Imagination Library and the Communities Supporting Early Literacy initiative continued in these same communities, leveraging relationships and coalitions to continue to improve early literacy and lifelong learning.
KHF has also dedicated $8.4 million to its Kansas Healthy Food Initiative, a loan/grant effort to improve access to healthy foods in neighborhoods and communities that are food insecure. The challenge with food insecurity is that it affects rural and urban communities, where people have to drive or walk long distances to find fresh and/or healthy food options.
Where To Go From Here
KHF supports health policies that reduce disparities and promote health equity (in access and participation) by income, race and ethnicity, and geographic location. It also supports reducing barriers for underserved populations, especially as it comes to access to care, digital connectivity (broadband and affordable access), supporting education needs with remote learning and expanding economic opportunities for families and businesses.
Sometimes this means working with partners to reduce barriers of historically disenfranchised communities to vote, access health care and receive information in a language they understand. In other situations, it may require collaborative advocacy for sustainable healthy policy change, including efforts for new rural health care models.
Often times, the most important aspect of health equity work is engaging directly with populations and creating culturally-appropriate strategies. Through these relationships and trusted community connections, we are able to reach those most in need.
As we continue through this year, KHF will be working to further define health equity with our next strategic plan, establishing the goals and health policy priorities to help measure how our resources will continue to reduce inequities.
Be watching our website and sign up for our e-newsletters (you can do so in the box below marked “Sign Up for KHF’s Electronic Newsletters”) to learn more about health equity and the impact certain inequities have on our state and nation.